 Home Screen
Home Screen Home Screen
Home Screen
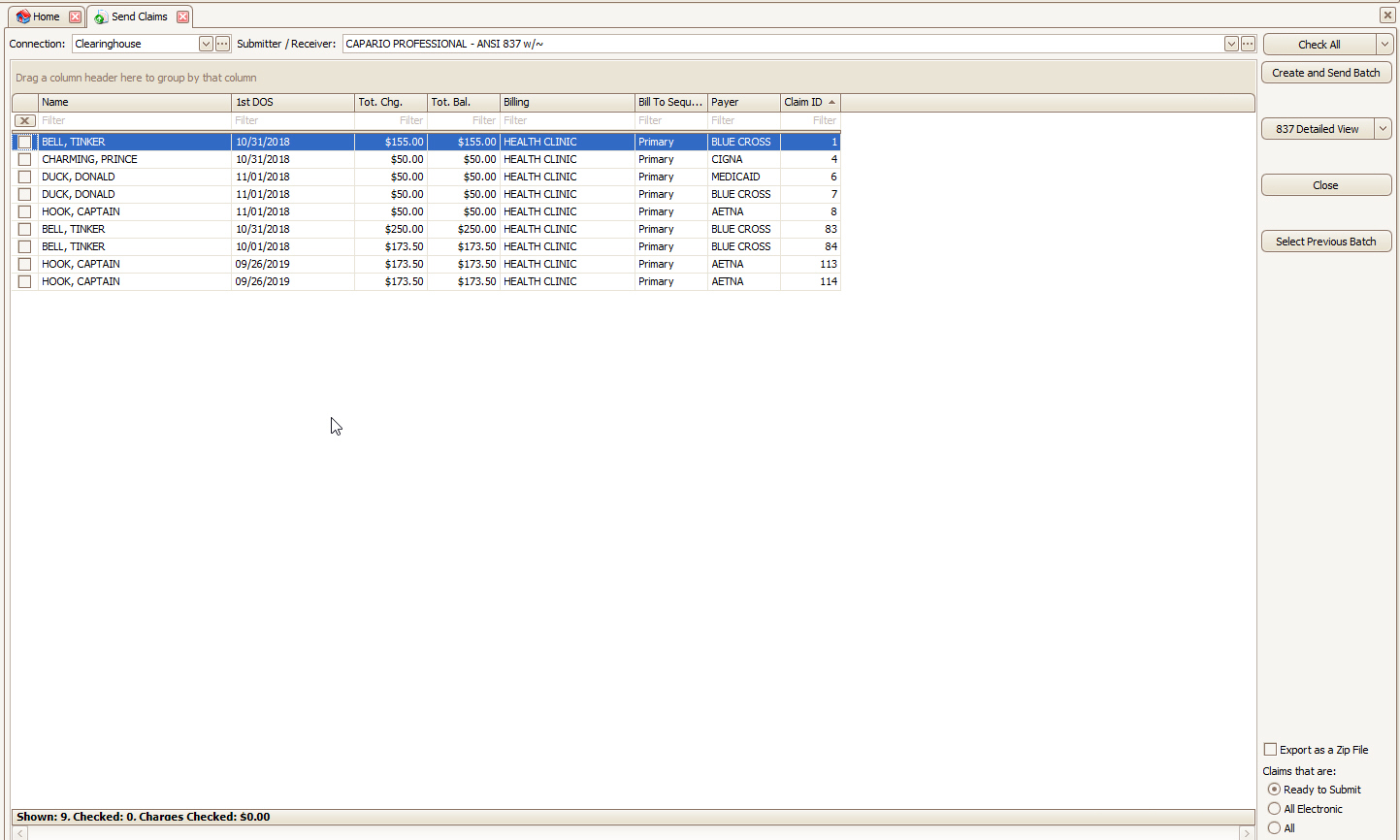
The ‘Send Claims’ screen is used for electronic claim submission. It allows the user to batch claims, generate a file, and submit the file electronically to a Payer or Clearinghouse. The Submitter/Receiver Library allows you to store file transmission specifications (ANSI 837 file headers and loops) as required by the Payer or Clearinghouse receiving your data.
Clicking the ‘Send Claims’ button from the ‘Home’ screen will open the ‘Send Claims’ dialog box listing claims ready for electronic submission (EDI).
Claims Missing from the List?
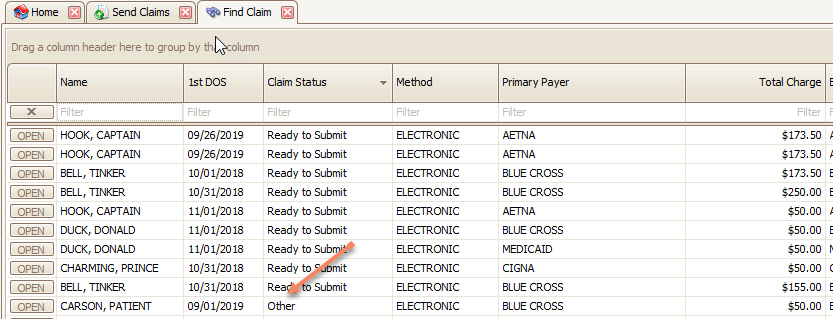
If claims are not appearing in this grid, it means they are being filtered out in some way. Please go to your Home > Find > Find Claim and confirm the following:
•Is Claim Status set to Ready to Submit? In the example below, the Claim Status ‘Other’ would filter the claim from the grid.
•Is the Claim Method set to Electronic?
•Is Bill To (or Resp. Party at the service line level) on the “missing” claim currently set to Patient? This will prevent the claim from being seen as sendable by Premier.
•If you submit both Professional and Institutional claims, are you selecting the appropriate Submitter/Receiver Library entry? If so, have you selected the correct Claim Type in the Payer Library entry?
•Is any grid field (e.g., Primary Payer) currently filtered? If so, right click the column heading and select ‘Clear Filter’.
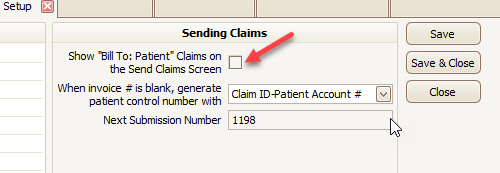
Unwanted Claims Appearing on the List?
Go to Tools > Program Setup > Sending Claims, then uncheck the following box:
A reference guide for the ANSI 837 Professional specifications is available online.
The Connection drop-down selection determines how the batch file is handled once the file has been created.
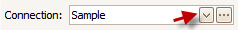
‘Just Export File’ allows you to save the file to your computer desktop or drive. Additional connection types determine how the file will be batched to send to the Payer or Clearinghouse. See EDI Connection Library for setting up your Connection Library.
The Submitter/Receiver drop-down allows you to select the Payer information previously set up in the Submitter/Receiver Library and includes the ANSI 837 header information, ISA, GS, Loop 1000A and Loop 1000B. See Submitter/Receiver Library for setting up the Submitter/Receiver Library.
Only claims which have been checked will be included in the batch. Select claims individually or use the ‘Check All’, ‘Uncheck All’, ‘Check Selected’, or ‘Uncheck Selected’ buttons to check claims.
If you need to resubmit a batch of claims sent previously, click ‘Select Previous Batch’ and highlight the previous submission.
See Resending Batches for re-submitting previous batches of claims.